Psychedelics & Pain
Pain is a complex and active ecology.
There is no single definition or manifestation of pain or chronic pain.
Pain can be both a symptom and a disease.
Primary pain is a disease unto itself (ie: migraine, cluster headache, CRPS). Secondary pain is a symptom resulting from another disease process or nervous system dysfunction (ie: peripheral neuropathy in diabetes, phantom limb pain, post-surgical pain). In some cases, secondary pain can maladaptively transition to primary pain (e.g. pain from spinal injury persisting past the healing period). This is where psychedelic medicines may be helpful in resetting and reducing pain.
Chronic pain serves no survival function in some circumstances.
Pain output, or intensity, should be a short term “alarm” aimed at preserving life. With chronic pain, this intensity can persist well beyond healing, deeply degrading quality of life and serving only maladaptive purposes.
Some pain is a perception.
Some pain can persist long enough to generate structural changes in our processing networks, so overwhelming them with signal that any input (ie. stimulation) can cause the central nervous system to fire off pain pathways. In this way, normal reflexes can become maladaptive and painful.
Pain is highly contextually dependent and can be a neurological disorder in and of itself.
We each experience pain differently — an extreme pain for you might be a minor bother for another. Pain has both external and internal (think: psychological) factors that can modulate the felt intensity of pain perception. Some pain (like migraine, CRPS, or cluster headache) can be entirely “organic,” non-injurious disorders of the nervous system. Likewise, these types of pain may develop subsequent to injury or surgery and represent pure neurological dysfunction.
Some pain exists in the total absence of injury, disease, or in the post-recovery period when healing is “complete.”
Extremely prevalent, fibromyalgia is an example of pain signals firing when no “injury” is present. In fibro, the normal aches and pains of daily life, most commonly resolved with movement, become chronic, exaggerated, and debilitating. Whatsmore, this type of pain can gather features bodywide, taking on new characteristics: cognitive deficits, depression, gut impairment, etc.
We need updated models for addressing pain.
Previous pain models do not fully address the complexity of pain, nor the differences in severity, duration, & scope from one individual to another, even with the same pain condition.

Cartesian Model
Developed in the 1600s, assumed that all pain symptoms were the result of tissue damage.

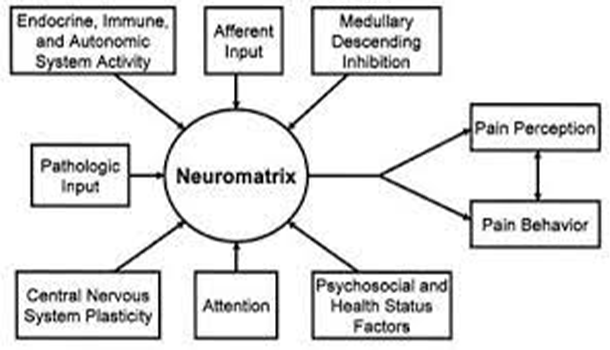
Pain Neuromatrix Model
These neurosignature patterns may be triggered by sensory inputs.

Bio-Psycho-Social Model
This model of pain is more comprehensive including psychological and social aspects.
Cartesian Model
The Cartesian model, developed in the 1600s, assumed that all pain symptoms were the result of tissue damage and that there was an organic explanation for all symptoms. It assumed a proportionate amount of pain relative to injury or disease.
Critique: It is incorrect to assume that pain is simply a sensation received from the peripheral nerves (e.g.g at an injury site) ascending to the brain. This model does not account for medically unexplained symptoms because it is looking for acute pain causes that can be treated and resolved.

Pain Neuromatrix Model
Pain Neuromatrix model proposes that pain is a multidimensional experience produced by “neurosignature” (each individual’s unique, neurological “combination lock” that creates pain specific to them) patterns of nerve impulses generated by a widely distributed neural network, the “body-self neuromatrix” in the brain. These neurosignature patterns may be triggered by sensory inputs, but they may also be generated independently of them.
The Pain Neuromatrix model proposes that pain is a complex experience produced by a “neurosignature” (each individual’s unique pattern of nerve impulses that creates pain specific to them) generated by a widely distributed neural network between the brain and the sensory system (ie. the parts of the body that “feel”), what is referred to as the “body-self neuromatrix”.
These neurosignature patterns may be triggered by sensory inputs, but they may also be generated independently of them.
Critique: The neuromatrix model of pain portrays the complex intertwining of different areas of our nervous system, mind, and body and the influence this has on pain and pain perception.

Bio-Psycho-Social Model of Pain
This model of pain is more comprehensive including psychological and social aspects that have been documented to have an impact on perceptions of pain.
Critique: Too often this model is used by the medical system to direct patients towards psychological and social treatments for pain without providing appropriate support. Healthcare providers or insurance companies sometimes don’t prescribe or cover treatments for biological causes of pain.

Psychedelic Medicine for Pain
Psychedelic medicines will play a role in expanding the scope of treatment and understanding of complex pain.
Psychedelics are powerfully effective via their neurological mechanisms of action in treating chronic pain AND they can also address other key intrinsic factors: psychological & social contributors that strongly influence the intensity of pain perception and output as we now understand them through the Bio-Psycho-Social and Pain Neuromatrix model.
Key Mechanisms of Action
The complexity of pain is well matched by the multiple and complex ways that psychedelic substances can impact human physiology and perception. Psychedelic medicines have a number of biological effects that can reduce or prevent pain, such as the anti-nociceptive and anti-inflammatory impacts that many studies have identified. Psychedelics can also create neuroplasticity that enables people to alter and improve their relationship to the pain they experience.
New mechanisms of action for how psychedelics improve pain are continually being discovered and proposed. Mounting evidence seems to show that a confluence of biological, psychological, and social factors contribute to the potential of these medicines to treat complex, chronic pain. It is premature to state that there is one key or overarching mechanism. We support continued research to explore different ways that various psychedelics impact the wide range of pain conditions.
Below is a summary of the key mechanisms of action that are currently proposed for how psychedelics reduce pain and suffering. These concepts are presented discretely for clarity – but they almost certainly occur concurrently, interact dynamically and have impact synergistically.
Experience Mediated / Psychological Reframing
This pared down state may allow individuals to distance themselves from identification with pain, disability, and demoralization…
Thalamic Gating
The thalamus is a critical structure in processing noxious (harmful, unpleasant) input and regulating pain output…
5-HT2A Gene Polymorphisms
Research suggests that psychedelics may treat chronic pain by targeting, and activating, the 5-HT2A receptor…
Modulating Functional Connectivity in the Brain
Brain functional connectivity (FC) refers to the patterns of communication between different brain regions and structures…
Modulating Gene Expression
Psychedelics may treat chronic pain by modulating gene expression, either by decreasing or increasing expression, or activation, of certain genes…
Modulating Inflammation
Recent studies in animal models have shown the remarkable potential of psychedelic medicines to normalize body-wide levels of inflammation and to modulate the immune response…
Inhibitory 5HT Pathways
Psychedelics may turn on the body’s natural pain-relieving function by activating descending inhibitory 5HT (serotonin) pathways…
Inhibitory 5HT Pathways
Psychedelics may turn on the body’s natural pain-relieving function by activating descending inhibitory 5HT (serotonin) pathways — a series of nerves that descend from the midbrain and brainstem to the spinal cord. These nerves help control how the spinal cord responds to pain signals and it is hypothesized that malfunction in these nerve pathways can lead to the development of inappropriate pain patterns, such as “hyperalgesia” (increased sensitivity to pain) and “allodynia” (pain coming from stimulus that normally would not cause pain). In a study using rat models, these 5HT nerve pathways were tied off to explore if nerve signals could persist past nerve injury; only the 5HT2A receptor pathways were able to continue pain inhibition persistently. This is significant because the 5HT2A receptor is the central target of most classic psychedelics suggesting that psychedelic medicines may play a role in pain management subsequent to a variety of nerve injuries.
Liu F-Y, Qu X-X, Ding X, et al. Decrease in the descending inhibitory 5-HT system in rats with spinal nerve ligation. Brain Res 2010;1330:45–60.
Obata H, Saito S, Sakurazawa S, et al. Antiallodynic effects of intrathecally administered 5-HT2C receptor agonists in rats with nerve injury. Pain 2004;108:163–9.
Sasaki M, Obata H, Saito S, et al. Antinociception with intrathecal alpha-methyl-5- hydroxytryptamine, a 5-hydroxytryptamine 2A/2C receptor agonist, in two rat models of sustained pain. Anesth Analg 2003;96:1072–8.
Modulating inflammation
Recent studies in animal models have shown the remarkable potential of psychedelic medicines to normalize body-wide levels of inflammation and to modulate the immune response.
Using the psychedelic (R)-DOI mouse and rat models have displayed a potent reduction in the master inflammatory cytokine TNF-alpha, thereby regulating the inflammatory response in asthmatic and cardiovascular inflammatory models. While still in preclinical stage, these models may act as powerful proxies for the potential of these medicines to bring inflammatory biomarkers back to homeostatic (i.e. healthy) levels across a wide range of conditions.
Further research is demonstrating the ability of classic psychedelics (e.g. psilocybin, LSD, DMT) to inhibit secretion of additional inflammatory cytokines, namely IL-1b and IL-6 and even to increase anti-inflammatory cytokines, like IL-10.
Finally, the potential of the psychedelic experience to modulate psychological stressors plays a part in the reduction of body-wide inflammation. It has been well established that mental-emotional stress, such as in depression or PTSD, increase peripheral cytokine concentration and therefore inflammation.
Profound, or even mystical, experiences on psychedelics may induce a reduction in inflammation through their ability to modulate reactivity to psychological stressors. It has been well established that mental-emotional stress, such as in depression or PTSD, increases peripheral cytokine concentration and therefore, inflammation. The easing of the stress response subsequent to use of psychedelics may then play an indirect role in the overall normalization of inflammation we see in research subjects and anecdotally.
Thomas W. Flanagan & Charles D. Nichols (2018) Psychedelics as anti-inflammatory agents, International Review of Psychiatry, 30:4, 363-375, DOI: 10.1080/09540261.2018.1481827
Mason NL, Szabo A, Kuypers KPC, Mallaroni PA, de la Torre Fornell R, Reckweg JT, Tse DHY, Hutten NRPW, Feilding A, Ramaekers JG. Psilocybin induces acute and persisting alterations in immune status in healthy volunteers: An experimental, placebo-controlled study. Brain Behav Immun. 2023 Nov;114:299-310. doi: 10.1016/j.bbi.2023.09.004. Epub 2023 Sep 7. PMID: 37689275.
Modulating Gene Expression
Psychedelics may treat chronic pain by modulating gene expression, either by decreasing or increasing expression, or activation, of certain genes. By activating the 5-HT2A receptors (found across the body, including nerve cells, immune cells, and cells in the gut) psychedelics may decrease the expression of genes that produce pain signals and make certain people more susceptible to inappropriate pain patterns. As an example, it has been observed that activation of the 5HT2A receptors, through the use of psychedelics, can increase the release of brain-derived neurotrophic factor (BDNF). BDNF is a protein that plays a crucial role in nerve growth and repair, and is thought to have anti-inflammatory effects. Not limited to the 5HT2A receptors, these medicines likewise modulate gene expression through interaction with other receptor sites, namely cannabinoid and sigma-1 receptors. Like the 5HT2A receptors, these are also involved in pain processing and inflammation.
Pei Q, Lewis L, Sprakes ME, et al. Serotonergic regulation of mRNA expression of Arc, an immediate early gene selectively localized at neuronal dendrites. Neuropharmacology 2000;39:463–70.
Benekareddy M, Nair AR, Dias BG, et al. Induction of the plasticity-associated immediate early gene ARC by stress and hallucinogens: role of brain-derived neurotrophic factor. Int J Neuropsychopharmacol 2013;16:405–15.
Modulating Functional Connectivity in the Brain
Brain functional connectivity (FC) refers to the patterns of communication between different brain regions and structures. Mounting evidence shows many pain conditions, similarly to psychiatric disorders, FC in the brain is altered, essentially locking individuals into maladaptive chronic pain states that serve no survival function. The central nervous system (CNS) is constantly involved in top-down predictive processing, threat assessments of the external and internal environment, and then error correcting those predictions via bottom-up sensory stimuli. These predictions reinforced over time become “strong priors”, becoming default responses or frameworks. But they can also start suppressing bottom-up error correction and allow maladaptive priors to become entrenched and predominate.
The incredible potential for psychedelics to interrupt established FC patterns could allow for more plasticity, or adaptability, of the brain, acting like a “reset” to disruptive pain patterning by favoring bottom-up sensory processing and flattening the strong priors in the cortical landscape, “relaxing” them. This disruption of FC patterns may be therapeutic for chronic pain by breaking down dysfunctionally entrenched pain pathways during the “chaotic” brain-state of psychedelics, allowing new, functional connections to form in their place, after creating a more plastic, adaptable brain state. It is this increased plasticity while under the influence of psychedelics that appears most promising when combined with adjunctive modalities such as physical therapy, mirror-visual-feedback, neuromodulatory techniques, bodywork, and more.
This plasticity is achieved due to increases in neuritogenesis, synaptogenesis, dendritic arborization and complexity, and spinal trunk thickness. While not causing the growth of new neurons, these neuronal structure improvements are like a forest of trees blooming in springtime receiving nutrients and sunlight, sprouting new branches and leaves, growing a thicker trunk, and fostering connections with other trees through an invigorated and broadened root-system.
All of this is likely promoted in part by psychedelics causing a release of BDNF, brain-derived neurotrophic factor, causing these improvements in neuronal structures and connectivity. BDNF also co-regulates glutamate, a major excitatory neurochemical messenger in the cortex, which also can play a prominent role in pain modulation.
Zhang S, Wu W, Huang G, et al. Resting-State connectivity in the default mode network and insula during experimental low back pain. Neural Regen Res 2014;9:135–42.
Li C-T, Chen L-F, Tu P-C, et al. Impaired prefronto-thalamic functional connectivity as a key feature of treatment-resistant depression: a combined MEG, PET and rTMS study. PLoS One 2013;8:e70089.
Carhart-Harris RL, Leech R, Hellyer PJ, et al. The entropic brain: a theory of conscious states informed by neuroimaging research with psychedelic drugs. Front Hum Neurosci 2014;8:20.
5-HT2A Gene Polymorphisms
Research suggests that psychedelics may treat chronic pain by targeting, and activating, the 5-HT2A receptor. This receptor is involved in pain processing, and over-activation of the receptor can lead to chronic pain. Some people have gene variations (“polymorphisms”) on the 5-HT2A gene, which can make them more susceptible to chronic pain conditions such as fibromyalgia, chronic widespread pain, and pelvic pain. It is hypothesized that those with these polymorphisms may be more sensitive to the activation of 5-HT2A receptors by psychedelic medicines, thus decreasing inflammation, sensitivity to pain, and promoting neuroplasticity.
Bondy B, Spaeth M, Offenbaecher M, et al. The T102C polymorphism of the 5-HT2A-Receptor gene in fibromyalgia. Neurobiol Dis 1999;6:433–9.
Nicholl BI, Holliday KL, Macfarlane GJ, et al. Association of HTR2A polymorphisms with chronic widespread pain and the extent of musculoskeletal pain: results from two population-based cohorts. Arthritis & Rheumatism 2011;63:810–8.
Thalamic Gating
The thalamus is a critical structure in processing noxious (harmful, unpleasant) input and regulating pain output. As a key relay station or “hub”, the thalamus manages sensory and cognitive signals throughout the brain, while “gating” (ie. filtering out), the vast majority of sensory input, so that we are able to perform day to day functioning without being overwhelmed. Under psychedelics, that tight regulation is significantly inhibited, allowing a flood of both external and internal sensory inputs to reach the cortex, creating the classic psychedelic “mystical” experience.
Pain output is modulated with descending inhibition and the thalamus receives nociceptive sensation via ascending spinal pathways and from multiple brain circuits carrying the affective-emotional components of pain perception, how we feel about the pain we’re experiencing. All of these structures and pathways critical to our experience of pain have 5HT2A receptors throughout — it is hypothesized that classic psychedelics have a regulatory interaction in thalamic pain modulation, and thereby the ability to modulate or decrease our sensation of pain.
Functional Connectivity
Brain functional connectivity (FC) refers to the patterns of communication between different brain regions and structures. Mounting evidence shows that in many pain conditions, similarly to psychiatric disorders, FC in the brain is altered, essentially locking individuals into maladaptive chronic pain states that serve no survival function.
The remarkable potential for psychedelics to interrupt established FC patterns could allow for more plasticity, or adaptability, of the brain, acting like a “reset” to disruptive pain patterning by favoring bottom-up sensory processing and flattening the strong priors (i.e. entrenched maladaptive pain patterns) in the cortical landscape, “relaxing” them. This disruption of FC patterns may be therapeutic for chronic pain by breaking down dysfunctional pain pathways during the “chaotic” brain-state of psychedelics, allowing new, functional connections to form in their place, after creating a more plastic, adaptable brain state. It is this increased plasticity while under the influence of psychedelics that appears most promising when combined with adjunctive modalities such as physical therapy, mirror-visual-feedback, neuromodulatory techniques, bodywork, and more.
This plasticity is achieved due to increases in neuritogenesis, synaptogenesis, dendritic arborization/complexity, and spinal trunk thickness. While not causing the growth of new neurons, these neuronal structure improvements are like a forest of trees in springtime, receiving nutrients and sunlight, sprouting new branches and leaves, growing a thicker trunk, and fostering connections with other trees through an invigorated and broadened root-system.
All of this is likely promoted in part by psychedelics causing a release of BDNF, brain-derived neurotrophic factor, causing these improvements in neuronal structures and connectivity. BDNF also co-regulates glutamate, a major excitatory neurochemical messenger in the cortex, which also can play a prominent role in pain modulation.
Zhang S, Wu W, Huang G, et al. Resting-State connectivity in the default mode network and insula during experimental low back pain. Neural Regen Res 2014;9:135–42.
Li C-T, Chen L-F, Tu P-C, et al. Impaired prefronto-thalamic functional connectivity as a key feature of treatment-resistant depression: a combined MEG, PET and rTMS study. PLoS One 2013;8:e70089.
Carhart-Harris RL, Leech R, Hellyer PJ, et al. The entropic brain: a theory of conscious states informed by neuroimaging research with psychedelic drugs. Front Hum Neurosci 2014;8:20.

Experience Mediated/Psychological Reframing
In the chronic pain state, one’s perception of sensation becomes maladaptively altered, making some aspects overly intense and others diminished, distorting the usual comprehensive picture we rely on for correct bodily information and threat assessment. When entering a deep psychedelic state or undergoing other profound experiences, layers of perception are stripped away, revealing the fundamental way the brain constructs one’s reality. This pared down state may allow individuals to distance themselves from identification with pain, disability, and demoralization, consequently “reframing” their relationship to pain. This can lead to a reduction in emotional suffering and PTSD comorbid with pain, as well as a loosening of their identification with being a person with chronic pain.
Two main models have been proposed to explain the “experience-mediated” or “reframing” effects of psychedelic medicine. Both involve complex interactions between the substance, the individual’s brain, and their subjective perceptions, likely involving all of the mechanisms of action listed here but are often discreetly organized, affording nuanced description.
In the REBUS model from Carhart-Harris & Friston it is posited that during the entropic state engendered with psychedelics, the brain has a chance to create more equilibrium between the somatic (feeling) and the cognitive (thinking) aspects of one’s experience, allowing for more accurate predictions about, and reactions to, the world and self. In the case of chronic pain, this allows for a re-weighting, or resetting, of the “strong priors” that the brain has established for efficiency, but that maladaptively keep an individual in a state of chronic pain, unrelated to actual threats.
The critical period reopening model, proposed by Dölen and colleagues, refers to a specific developmental window during which the brain is particularly sensitive to environmental stimuli, and neural circuits are more susceptible to modification. It was previously believed that this critical period was incredibly narrow and unable to “reopen” after neurological development early in life. However research has shown that psychedelic medicine has the potential to temporarily alter brain function, leading to increased plasticity and potentially reopening critical periods. For those with chronic pain, this reopening may allow the brain to reorganize around pain states, bringing the individual to more realistic expression of sensation and thereby, less pain.
Nardou, R., Sawyer, E., Song, Y.J. et al. Psychedelics reopen the social reward learning critical period. Nature 618, 790–798 (2023). https://doi.org/10.1038/s41586-023-06204-3
Modulation of Descending Inhibitory 5HT Pathways
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur. Excepteur sint occaecat cupidatat non proident, sunt in culpa qui officia deserunt mollit anim id est laborum.
Bringing Inflammation Back to Homeostasis
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur. Excepteur sint occaecat cupidatat non proident, sunt in culpa qui officia deserunt mollit anim id est laborum.
Downstream Effects: Modulation of Gene Expression
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur. Excepteur sint occaecat cupidatat non proident, sunt in culpa qui officia deserunt mollit anim id est laborum.
Specific 5-HT2A Gene Polymorphisms
Lorem ipsum dolor sit amet, consectetur adipiscing elit, sed do eiusmod tempor incididunt ut labore et dolore magna aliqua. Ut enim ad minim veniam, quis nostrud exercitation ullamco laboris nisi ut aliquip ex ea commodo consequat. Duis aute irure dolor in reprehenderit in voluptate velit esse cillum dolore eu fugiat nulla pariatur. Excepteur sint occaecat cupidatat non proident, sunt in culpa qui officia deserunt mollit anim id est laborum.
Inflammation, Autoimmunity, & Psychedelics
[Under Construction…]
